I represent the little guy — civil rights plaintiffs, whistleblowers, consumers and inmates, to name a few.
My opposition is often BigLaw firms, the ones with hundreds, if not thousands, of lawyers.
On a normal day, I have my disputes with these firms over pleading standards, compulsory arbitration and deference to administrative agencies. We battle it out within the legal system. It’s an imperfect system, no doubt, affected by politics and bias.
I didn’t think I’d ever advocate on behalf of these firms. But today, I feel compelled to do so, because of an issue that affects us both — the executive orders targeting some of the nation’s largest law firms.
This isn’t just about BigLaw, and it’s not just about the BigLaw firms named in executive
orders. It’s also about the small firms, the solo practitioners and the public interest lawyers who see what is happening to these big firms and are wondering what they will do if and when they, too, are targeted.
Make no mistake: If BigLaw firms can be targeted, so too can midsize law firms, boutiques, solo practitioners, prosecutors and public defenders. Though I litigate against BigLaw, on this day and on this matter, we are kindred spirits.
The legal system only works if lawyers can represent clients without retribution or fear of retribution. Once in court, advocacy is regulated by the tribunal itself.
Ethical, procedural and evidentiary rules govern the lawyer and the process. It is a laboratory environment where, on a good day, a case will sink or swim on the merits, and the lawyers will move on to the next matter untainted by their advocacy on behalf of an entity or person whose position did not prevail or whose conduct was deemed unsavory.
In addition to the orders targeting specific law firms, the president signed a memorandum on March 22 making it clear that none of this is limited to just a few large firms. That memo directs the attorney general to be more aggressive in the use of sanctions motions and ethical charges against those who litigate against the government. The memo states:
I further direct that, when the Attorney General determines that conduct by an attorney or law firm in litigation against the Federal Government warrants seeking sanctions or other disciplinary action, the Attorney General shall, in consultation with any relevant senior executive official, recommend … additional steps that may be taken, including reassessment of security clearances held by the attorney or termination of any Federal contract for which the relevant attorney or law firm has been hired to perform services.1
The March 22 memo is noteworthy not only for what it says but for what it does not say. It provides for a referral for “additional steps,” including the loss of contracts or the loss of security clearance, not after a court determines that sanctions are warranted, but after the attorney general makes such a determination. That referral can occur without a motion for sanctions being filed, or before the court has ruled on a motion for sanctions. Under this memo, the referral and additional steps can be taken even if the court denies the motion for sanctions.
It is, in sum, a memo that provides a litigant — indeed the defense counsel for the government and the government itself — the sole right to sanction counsel. In this way, the memo effectively removes the judge from the sanctions calculus.
The sanction of having security clearance withdrawn is of course not an abstract proposition. A lawyer needs security clearance to represent, for instance, employees of the CIA, the FBI and the intelligence community who have lost their jobs through Department of Government Efficiency cutbacks. And a number of the firms representing plaintiffs in these cases are boutique or midsize litigation firms, or public interest nonprofits.
By eliminating the security clearance of lawyers or maintaining a threat to do so, a defendant — in this case the government — may essentially curtail opposing counsel’s ability to represent such clients, or influence their advocacy.
It was in Marbury v. Madison that Chief Justice John Marshall in 1803 famously said that “the very essence of civil liberty certainly consists in the right of every individual to claim the protection of the laws, whenever he receives an injury.”
Fundamental to that protection is the ability to secure counsel. There is no question that the March 22 memo will cause all lawyers — but especially public interest lawyers and solo practitioners — to think twice about whether to take on cases they would ordinarily assume.
Yes, the big firms have their pro bono practices, but it is the smaller firms and the boutique practices that tend do the everyday work of challenging government action. It is the small firms and public interest organizations whose institutional missions focus primarily on things like representing immigrants facing deportation or inmates of for-profit prisons who seek proper medical care, or bringing suits under the Freedom of Information Act to make government more transparent.
But these firms simply do not have the resources or cash flow of the big firms. Unlike Perkins Coie LLP, WilmerHale and Jenner & Block LLP, which have all challenged these executive orders, small firms may be unable to tap the expertise of the best constitutional lawyers in the land to defend themselves against ruin.
Imagine a scenario where a solo practitioner represents a student who is in this country under a student visa, but who has been detained and subject to deportation because of the content of an article they authored in the student newspaper. How might that practitioner react when the government lawyer takes him aside and says that a potential lawsuit is sanctionable? A gutsy lawyer might say, “I’ll see you in court.” But of course, under the March 22 memo, the government may secure sanctions absent a court determination.
The sanctions might include loss of security clearance and/or loss of government contracts. For the lawyer who represents members of the intelligence community or the public interest group that benefits from government grants, the threat is significant. But these are only examples as the memo’s use of the phrase “additional steps that maybe taken, including” makes clear that potential recriminations are boundless.
A big firm may have lobbyists or insiders who can negotiate a resolution with the president. But the average solo practitioner does not have such access or leverage.
In the end, solo practitioners, small law firms and public interest attorneys may find themselves more dramatically affected by the collective impact of these executive orders and memoranda than even the BigLaw firms that have been directly targeted.
Absent the resources and revenue of their BigLaw counterparts, these firms may just temper their advocacy or curtail client relationships. When this happens, there will be no headlines or banner story on the nightly news. Public interest advocacy will have been curtailed — perhaps forever — in ways that will not be easy to quantify.
______________________________________
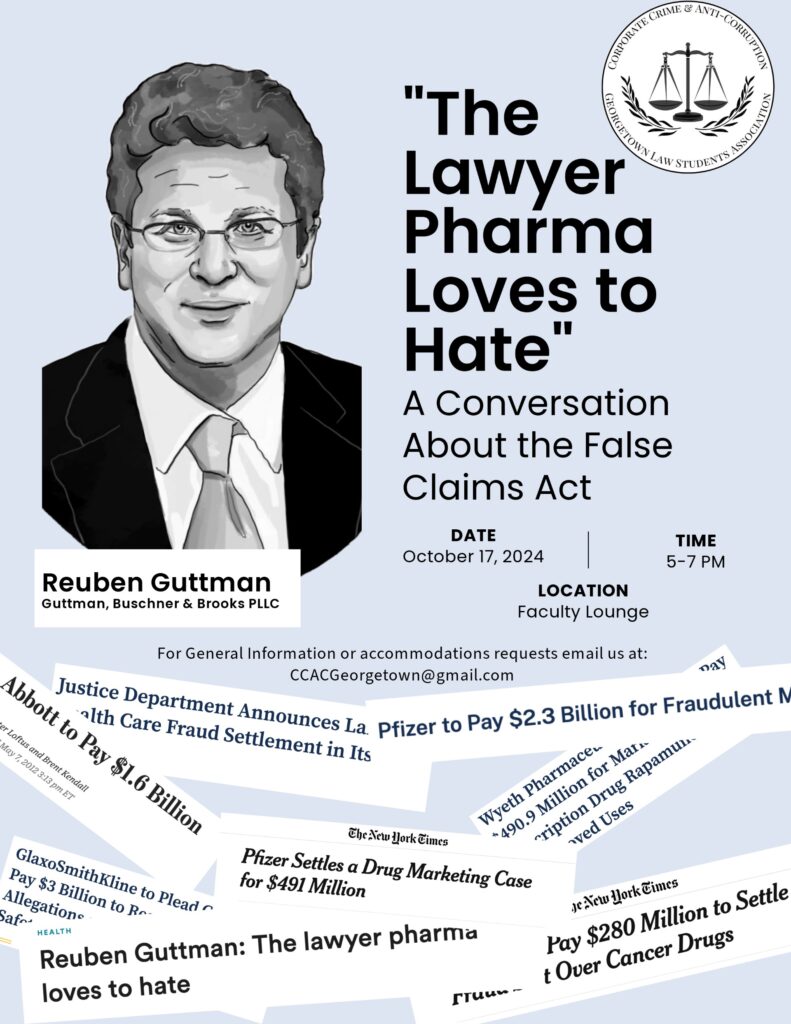
Reuben A. Guttman is a senior founding partner at Guttman Buschner & Brooks PLLC. The opinions expressed are those of the author(s) and do not necessarily reflect the views of their employer, its clients, or Portfolio Media Inc., or any of its or their respective affiliates. This article is for general information purposes and is not intended to be and should not be taken as legal advice.